How are autoantibodies diagnosed and treated today
Autoantibodies are crucial players in the realm of immunology, representing a significant aspect of our understanding of autoimmune disorders. Their formation stems from an atypical immune response where antibodies erroneously target the body's own tissues. This phenomenon not only complicates the identification of autoimmune diseases but also necessitates a comprehensive approach to diagnosis and treatment. As the prevalence of autoimmune diseases rises, so does the imperative for innovative methods to diagnose and manage conditions linked to autoantibody formation.
Current medical strategies rely on advanced diagnostic tools and therapeutic interventions to address the challenges posed by autoantibodies. These interventions are designed to mitigate the harmful effects that arise when the immune system mistakenly attacks its own cells. It is essential to understand both the formation of autoantibodies and their implications for various autoimmune diseases to develop effective treatment pathways. This article aims to explore how autoantibodies are diagnosed and treated today, shedding light on the multifaceted nature of these immune components and their role in health and disease.
Understanding Autoantibodies
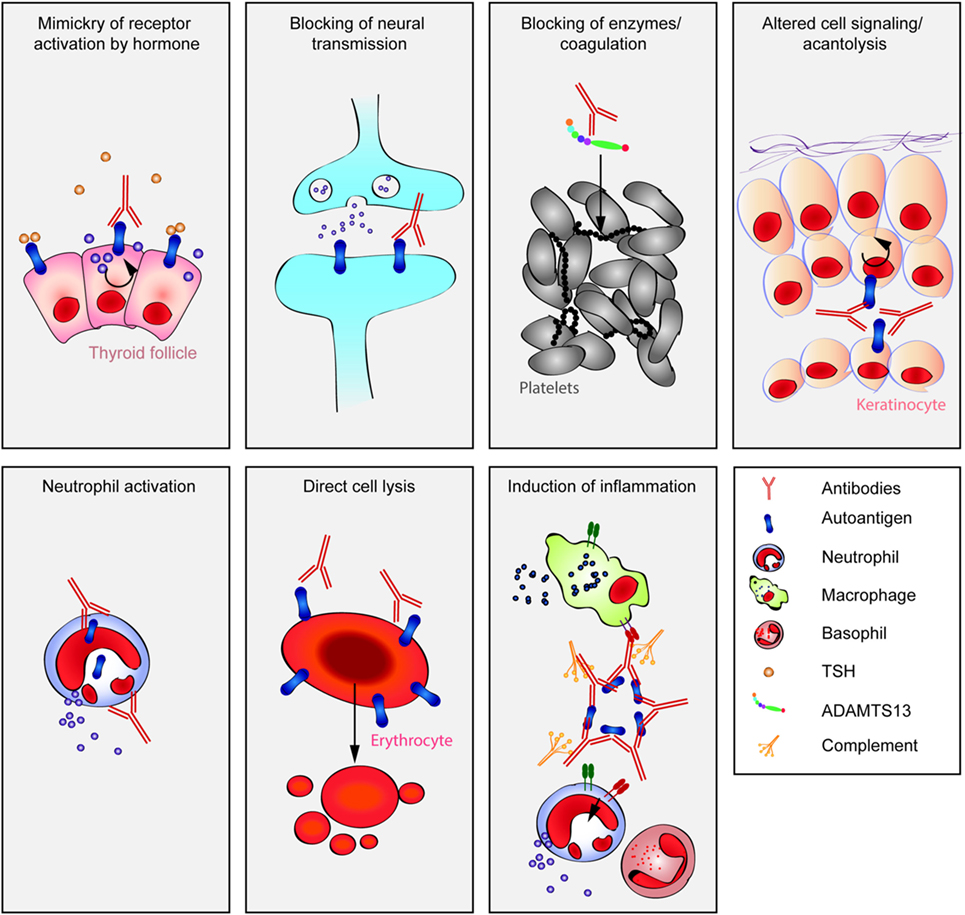
Autoantibodies are a subset of antibodies that the immune system produces against the body’s own proteins, also known as self antigens. The emergence of these autoantibodies can lead to a range of autoimmune diseases, where the body’s immune response becomes dysregulated. The specificities of autoantibodies can vary widely, with different types associated with various autoimmune conditions. Understanding the mechanisms behind their formation is crucial in grasping how they contribute to the pathogenesis of these diseases.
The Role of the Immune System
The immune system is designed to protect the body from foreign invaders, such as pathogens. However, its failure to distinguish between self and non-self antigens can result in the formation of autoantibodies. This aberration can lead to an attack on the body’s own cells, constituting the basis for autoimmune diseases. The autoantibody formation process involves various immune cells, including B lymphocytes, which are responsible for producing antibodies. When these cells are improperly activated, they may generate antibodies against the self antigens, leading to tissue damage and a range of clinical symptoms.
Common Autoimmune Diseases Associated with Autoantibodies
Many autoimmune diseases are characterized by the presence of specific autoantibodies. Some of the most common diseases include:
- Rheumatoid Arthritis (RA) - Associated with anti-citrullinated protein antibodies (ACPAs).
- Systemic Lupus Erythematosus (SLE) - Characterized by a wide array of autoantibodies, including antinuclear antibodies (ANAs).
- Graves’ Disease - Involves autoantibodies that stimulate the thyroid gland, causing hyperthyroidism.
- Hashimoto's Thyroiditis - Linked with autoantibodies that target thyroid peroxidase and thyroglobulin.
- Multiple Sclerosis (MS) - While not defined solely by autoantibodies, its pathogenesis can involve specific autoantibody responses.
Each of these diseases demonstrates unique forms of autoantibody formation that can lead to specific symptoms and clinical outcomes, highlighting the importance of understanding their implications.
Diagnostic Methods for Autoantibodies
Diagnosing diseases associated with autoantibodies requires a multifaceted approach. Clinicians use a combination of laboratory tests, imaging techniques, and clinical evaluations to confirm the presence of these autoantibodies and elucidate their impact on patient health.
Laboratory Tests and Their Significance
Laboratory tests are paramount in the diagnosis of autoimmune diseases. Commonly performed tests include:
- Antinuclear Antibody (ANA) test - Screens for the presence of various autoantibodies.
- Specific antibody tests - Such as anti-double-stranded DNA (anti-dsDNA) and anti-Smith (Sm) antibodies for SLE.
- Anti-citrullinated protein antibodies (ACPAs) - Indicative of rheumatoid arthritis.
The presence of specific autoantibodies can provide critical insight into the diagnosis and prognosis of autoimmune diseases. Elevated levels of these autoantibodies often correlate with disease activity, making them invaluable in both identifying the disease and monitoring treatment response.
Imaging Techniques in Diagnosis
In addition to laboratory tests, imaging techniques such as MRI and ultrasound can support the diagnosis of autoimmune diseases by visualizing the extent of inflammation and damage to affected organs. For instance, an MRI is commonly used to assess brain and spinal cord involvement in multiple sclerosis, while ultrasound can help evaluate joint inflammation in rheumatoid arthritis.
The Importance of Clinical Evaluation
A thorough clinical evaluation is essential in diagnosing autoimmune diseases. This evaluation typically includes:
- Patient history
- Symptom assessment
- Physical examination
Assessing these factors helps clinicians infer the likelihood of autoantibody formation and guides the choice of further testing. The culmination of laboratory and clinical findings ultimately shapes the diagnosis and informs treatment options.
Treatment for conditions associated with autoantibodies typically aims to reduce the immune response, alleviate symptoms, and minimize tissue damage. Strategies may include pharmacological and non-pharmacological approaches.
Immunosuppressive Therapies
Immunosuppressive therapies play a central role in managing autoimmune diseases by dampening the abnormal immune response that leads to autoantibody formation and tissue damage. Common medications include:
- Corticosteroids - Reduce inflammation and autoantibody production.
- Disease-modifying antirheumatic drugs (DMARDs) - Such as methotrexate, aimed at slowing disease progression.
- Biologics - Target specific components of the immune system.
These treatments can lead to significant improvements in patient outcomes by controlling inflammation and preventing the harmful effects of autoantibodies.
Targeted Biological Therapies
Targeted biological therapies represent an innovative approach to treating autoimmune diseases by specifically targeting pathways involved in autoantibody formation. For example, therapies like rituximab, which deplete B cells, have shown promise in diseases like rheumatoid arthritis and lupus. These therapies not only help in reducing autoantibody levels but also improve overall health outcomes.
Lifestyle Modifications and Supportive Care
In conjunction with medical treatments, lifestyle modifications play a crucial role in managing autoimmune diseases. Patients are encouraged to adopt:
- Anti-inflammatory diets - Rich in antioxidants and omega-3 fatty acids.
- Regular physical activity - To maintain joint function and overall health.
- Stress management techniques - Such as yoga and meditation.
These supportive care measures can enhance the effectiveness of treatment and improve the quality of life for individuals affected by autoantibody-related conditions.
Challenges in Diagnosis and Treatment
Despite advances in the understanding of autoantibodies, challenges remain in their diagnosis and treatment. For instance, the presence of autoantibodies does not always correlate with disease activity, complicating interpretations of laboratory results. Additionally, there is variability in how individuals respond to treatments, necessitating a tailored approach to therapy. Physicians must also navigate potential side effects of immunosuppressive therapies while ensuring optimal management of autoimmune conditions.
Future Directions in Research and Therapy
The field of autoimmune diseases is continuously evolving, with research focused on understanding the underlying mechanisms of autoantibody formation and developing more effective treatments. Future directions may include:
- Personalized medicine - Tailoring treatments based on genetic and molecular profiles of patients.
- Novel biomarkers - Identifying specific autoantibody profiles that can predict disease progression.
- Gene therapies - Exploring the potential of modifying the immune response at a genetic level.
Such advancements could not only improve diagnostic accuracy but also enhance treatment efficacy for autoimmune diseases associated with autoantibodies.
Conclusion
Understanding the dynamics of autoantibody formation is pivotal in the diagnosis and treatment of autoimmune diseases. As the field progresses, innovative diagnostic tools and treatment modalities continue to emerge, aiming to improve the lives of those affected by these complex conditions. By leveraging advanced laboratory tests, imaging techniques, and targeted therapies, healthcare providers are better equipped to manage the challenges posed by autoantibodies and their associated disorders. Continued research and clinical advancements hold the promise of a brighter future for patients living with conditions tied to autoantibodies.
Did you find this article helpful? How are autoantibodies diagnosed and treated today See more here Education.
Leave a Reply




Related posts